Office of the Corrections Ombuds, WA, Systemic Report - Mental Health Access & Services, 2021
Download original document:
Document text
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
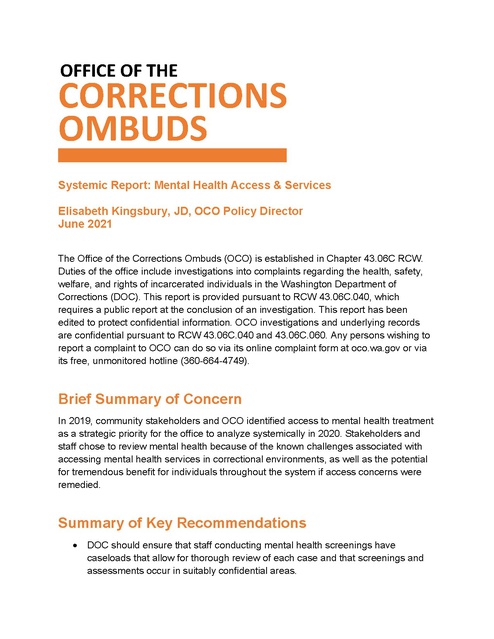
OFFICE OF THE CORRECTIONS OMBUDS Systemic Report: Mental Health Access & Services Elisabeth Kingsbury, JD, OCO Policy Director June 2021 The Office of the Corrections Ombuds (OCO) is established in Chapter 43.06C RCW. Duties of the office include investigations into complaints regarding the health, safety, welfare, and rights of incarcerated individuals in the Washington Department of Corrections (DOC). This report is provided pursuant to RCW 43.06C.040, which requires a public report at the conclusion of an investigation. This report has been edited to protect confidential information. OCO investigations and underlying records are confidential pursuant to RCW 43.06C.040 and 43.06C.060. Any persons wishing to report a complaint to OCO can do so via its online complaint form at oco.wa.gov or via its free, unmonitored hotline (360-664-4749). Brief Summary of Concern In 2019, community stakeholders and OCO identified access to mental health treatment as a strategic priority for the office to analyze systemically in 2020. Stakeholders and staff chose to review mental health because of the known challenges associated with accessing mental health services in correctional environments, as well as the potential for tremendous benefit for individuals throughout the system if access concerns were remedied. Summary of Key Recommendations • DOC should ensure that staff conducting mental health screenings have caseloads that allow for thorough review of each case and that screenings and assessments occur in suitably confidential areas. • DOC should ensure that quality, timely mental health treatment services are available to anyone in DOC custody who demonstrates a clinical need for treatment. • DOC should ensure that an individual’s mental health status is considered throughout the disciplinary process, including when reviewing infractions, determining guilt, and imposing sanctions. • DOC should develop comprehensive policies that address o Residential Treatment Units (RTUs) o Individual Behavior Management Plans (IBMPs) o Individuals in violator status • DOC should reduce the frequency of placement and length of stay in any segregated housing for individuals with mental health conditions. • DOC should provide additional mental health and de-escalation trainings to staff to increase positive and effective engagement with individuals who have mental health conditions. Special Considerations OCO recognizes the significant and unique ways in which mental health disorders impact Black, Indigenous, Latinx, and all people of color who are incarcerated. We urge readers to bear in mind our nation’s historical framework of racism and social injustice when considering the challenges faced by individuals with mental health conditions in prison, as discussed in this review. The experiences of incarcerated people with mental health disorders who identify as LGBTQIA+, women, and people with co-existing intellectual disabilities or other disabilities should also receive special consideration. OCO began consistently collecting demographic data for every complaint in 2020, and thus we do not have sufficient information to identify trends specifically related to race or other underserved populations in the complaints we received until that time. Anecdotally, however, OCO staff have noted concerning differences in the treatment of people of color with mental health disorders. OCO will continue to collect relevant data in order to better assess these concerns in the future. For now, we call upon DOC to make every effort to address the concerns identified in this report in ways that provide special attention to the impact on underserved populations. OCO Systemic Report: Mental Health Access & Services Page 2 Finally, the Covid-19 pandemic brought with it certain unprecedented challenges that must be acknowledged here. Undeniably, incarcerated individuals and prison staff throughout the nation and in our state have been profoundly impacted by the pandemic. OCO suspects that time may reveal lasting mental health effects for many individuals who endured months of quarantine and isolation. Presently, however, OCO has not observed any significant change in the types of complaints received from individuals who reported being on DOC’s mental health caseload; the concerns observed in 2019 related to treatment access persisted through 2020, but did not appear to intensify following the onset of the pandemic. We encourage DOC to remain vigilant about providing mental health support to all those individuals who endured and continue to endure quarantine and isolation due to Covid-19 restrictions. Scope of Review This report analyzed mental health complaints received by this office between November 2018 and November 2020. These complaints were identified by OCO staff as primarily involving a mental health concern at the time of intake. 1 Using data collected by OCO between November 2018 and November 2020, we identified approximately 335 complaints 2 that alleged difficulties accessing mental health treatment or other problems directly impacting or related to mental health. Having a mental health condition while incarcerated can result in exceptional difficulties beyond those already associated with incarceration. These include obtaining adequate treatment, disparate treatment, misperceptions and stigma, and increased vulnerability. This report primarily addresses access to treatment but additionally includes closely related concerns regarding the disciplinary system, segregated housing, and the roles and duties of mental health and custody staff. This report should not be considered an exhaustive list of all problems related to mental health that occur within DOC. OCO suspects many concerns go unreported for a variety of reasons, including obstacles such as incarcerated individuals’ fear of reprisal or limited ability to self-advocate. As stated above, the focus of this report is mental health treatment, as well as certain ancillary matters that often exacerbate individuals’ mental health conditions. This report Data specifically includes complaints tagged in OCO’s database with a mental health case factor as well as most complaints that reference “mental health” or “MH” in the case details. 2 Some complainants filed more than one complaint related to ongoing or new concerns. The data set we examined had 257 unique complainants. 1 OCO Systemic Report: Mental Health Access & Services Page 3 does not examine certain topics related to mental health which the office has investigated, or is investigating, separately. These include: • • • • • • Mental wellness concerns related to the impacts of Covid-19 quarantine and isolation (multiple reports published in 2020) Suicide and suicide prevention (multiple reports published in 2020; one report published in 2021) Single-person cell assignments due to post-traumatic stress disorder or other mental health condition (report published in 2021) Use of force and use of restraints on individuals experiencing mental health crises (forthcoming report on use of restraints) Gender dysphoria diagnoses and access to hormone replacement therapy (forthcoming report on systemic transgender concerns) Access to mental health services while participating in Therapeutic Community (forthcoming report on TC) Additionally, this report does not examine disorders frequently associated with mental health disorders, including: • • Intellectual disabilities, learning disabilities, or traumatic brain injuries Neurodevelopmental disorders, including attention deficit hyperactivity disorder and autism spectrum disorder Finally, this report identifies OCO’s primary concerns and recommendations regarding topics raised repeatedly in complaints filed with our office. These are meant to serve as overviews and should not be interpreted as being comprehensive examinations on any given topic. Statutory Authority Per RCW 43.06C.040, OCO has the authority to initiate “… an investigation upon his or her own initiative, or upon receipt of a complaint from an inmate, a family member, a representative of an inmate, a department employee, or others, regarding any of the following that may adversely affect the health, safety, welfare, and rights of inmates: (i) Abuse or neglect; (ii) Department decisions or administrative actions; (iii) Inactions or omissions; (iv) Policies, rules, or procedures; or OCO Systemic Report: Mental Health Access & Services Page 4 (v) Alleged violations of law by the department that may adversely affect the health, safety, welfare, and rights of inmates.” Investigative Actions OCO took the following actions in furtherance of this review: • • • • • • • • • • • • analyzed complaints of unmet needs of incarcerated individuals with mental health conditions received by OCO; surveyed incarcerated individuals; reviewed grievances related to mental health access and the responses provided by DOC; reviewed mental health records of incarcerated individuals; solicited input from outside stakeholders and community members; discussed concerns with DOC mental health staff members; discussed concerns and preliminary recommendations with DOC administration over the course of several months; reviewed nationwide best practices as identified by state and national organizations and scholars; analyzed states’ policies regarding mental health access for incarcerated individuals, including sister states of Oregon and Idaho; reviewed Washington DOC Health Plan; reviewed selected mental health training materials for new DOC employees; and reviewed DOC policies, including: o Mental Health Services (DOC 630.500) o Close Observation Areas (DOC 320.265) o Involuntary Antipsychotic Administration (DOC 630.540) o Disciplinary Sanctions (DOC 460.050) o Restrictive Housing (DOC 320.255) o Health Services Management of Alleged Sexual Misconduct Cases (DOC 610.025) Findings I. Screening & Assessment Mental health providers screening at intake have high caseloads and must conduct some screenings and assessments in areas where confidentiality is compromised. OCO Systemic Report: Mental Health Access & Services Page 5 • • • Mental health providers are responsible for processing an extremely high number of mental health screenings daily. Lack of suitably confidential areas for mental health screenings of individuals in reception/intake in some facilities. OCO has received complaints of lack of timely responses to kites requesting initial mental health assessments. II. Psychotherapy OCO has received numerous complaints from individuals who reported difficulty accessing mental health therapy. It should be noted that the majority of complaints received on this topic related to access, not quality, of services offered. Specific concerns about psychotherapy relayed to OCO include: • • • • • • • • Long wait time for accessing therapy. Lack of timely responses to kites requesting routine appointments. Lack of timely responses to kites when requesting help from mental health providers when in distress. Lack of variety of treatment options offered in smaller facilities; lack of access to treatment in lower-custody facilities. Lack of group therapy classes. 3 Lack of access to services because the individual does not have a diagnosed mental health condition, despite their desire to improve their mental wellbeing. 4 Lack of access to therapy following a traumatic event such as a staff assault. Lack of mental health therapy available through DOC while in work release. Despite the fact that individuals remain in DOC custody while in work release, DOC reports that mental health providers may propose evidence-based group therapy ideas to a committee for approval – Dungeons & Dragons is an example of one that has become popular and engaged people who otherwise might not have been open to therapy. Group therapy classes are led by a psychologist or other qualified mental health provider. Because providers’ caseloads are significant, groups are limited. 3 DOC reports that space is also a limiting factor. Particularly with older facilities, mental health providers often must use spaces outside of health services. The most significant limitation is that an officer must be assigned to wherever a group is held during the time at which it is held. DOC reports that it relies on volunteer-led groups to support individuals who do not have a clinical need for therapy but who find it beneficial to process challenges with another person who will listen. [DOC has confirmed that it does not have enough mental health providers to offer therapy to everyone who wants but does not have a medical need for therapy.] 4 OCO Systemic Report: Mental Health Access & Services Page 6 DOC does not provide mental health treatment to individuals in work release. The burden of arranging one’s own services in the community may be particularly significant for some individuals with mental health conditions, cognitive disabilities, and/or traumatic brain injury. III. Medication OCO has received numerous complaints from individuals who have alleged concerns related to psychiatric medication. • • • • • DOC prescriber decreased in dosage or discontinued psychiatric medications that the individual considered effective in the past. 5 DOC prescriber prescribed psychiatric medication(s) that the individual reports was/were previously ineffective. DOC prescriber discontinued psychiatric medications without counseling, planning, or proper titrating, resulting in individuals suffering significant withdrawal symptoms. 6 Delays in obtaining appointments with mental health prescribers. Lack of clear self-care criteria that an incarcerated individual might demonstrate when DOC is seeking an order for involuntary antipsychotic medication. DOC reports that certain medications – particularly Wellbutrin and Seroquel – may be misused and are therefore prescribed only as last resort options. 5 DOC also reports that individuals frequently are prescribed sedating medications while in jail prior to being received by WA DOC. DOC reports that, although people may desire to continue these prescriptions, DOC will not support continued use unless a corresponding diagnosis is present. DOC also reports that its formulary may differ from the formulary previously accessed by an individual, which could impact the medications available to that person. DOC reports that psychiatrist providers were instructed to ensure that an appointment with the patient occurs prior to discontinuation of any psychiatric medication. The volume of complaints received by OCO about this issue has decreased significantly since DOC addressed this concern in mid-2020. 6 OCO Systemic Report: Mental Health Access & Services Page 7 IV. Disciplinary Process The disciplinary process does not provide sufficient opportunity for the full consideration of a person's mental health condition when reviewing infractions, determining guilt, and imposing sanctions. 7 Specific complaints relayed to OCO include: • • Individuals receiving infractions for behaviors stemming from a diagnosed mental health condition. Sanctions given to individuals with active mental health conditions are excessive, meaningless, and/or ineffective in achieving behavior modification. In reviewing complaints on this topic, OCO has observed: • • Instances in which individuals with active symptoms of mental health disorders were not offered a department advisor to assist with a disciplinary hearing. Disciplinary policy does not provide specific guidelines about when a staff advisor should be appointed and when one must be appointed. Few instances in which it appeared that the hearing officer considered the mental health condition of the person at the time of the infraction for purposes of determining guilt or sanctions. V. Self-Harm & Close Observation Areas (COAs) Self-harm, suicide attempts, and death by suicide continue to be of great concern to OCO. OCO released a series of reports on deaths by suicide and suicide prevention in 2020. 8 Recently OCO published a report on our investigation of deaths by suicide that occurred during 2020. We reiterate the need to adopt and implement the recommendations included in those reports. DOC reports having developed a plan to implement a modified disciplinary pilot program in two Residential Treatment Units (the Special Offender Unit (SOU) at Monroe Correctional Complex and the Treatment and Evaluation Center (TEC) at Washington Corrections Center for Women). Modifications would focus on the appropriateness of sanctions, rather than guilt. DOC reports that this pilot program began at SOU and TEC in March 2021. 7 DOC has yet to respond to OCO's Overview Report on 2019 Suicides and/or implement certain recommendations. 8 OCO Systemic Report: Mental Health Access & Services Page 8 • • • • OCO has observed at least two instances in which an individual’s PULHESDXTR 9 R code, which indicates a history of self-harm or suicide attempt, was not updated following incidents of serious self-harm. OCO has been informed of incidents in which DOC staff did not create safety plans for individuals prior to their release from COA. OCO has been informed of a lack of a suitably confidential areas for interviewing individuals in COA in at least one facility. This concern was cited in at least one case as a reason why an individual’s safety plan had not been created. OCO has received complaints in which people have remained in COAs for extended periods of time, pending transfer. 10 VI. Residential Treatment Units (RTUs) Individuals seeking admission to a residential treatment unit (RTU) express concerns about the process and programming is limited in many RTU settings. • • OCO has received complaints from incarcerated individuals who had requested RTU-level care but had been denied admission. The reasoning behind the decisions related to admission, and to discharge, as well, is not always clear or transparent. 11 OCO has received complaints regarding the lack of programs, education, and activities available in all RTUs. Specifically, the need for a recreation aide in WCCW’s Treatment and Evaluation Center (TEC) program has been communicated to our office on multiple occasions. In 2019, DOC launched an internal workgroup to address concerns related to Residential Treatment Units. Multiple disciplines were represented within the workgroup members; custody and classification staff, psychology and psychiatry staff, facility administration, and headquarters staff participated. OCO and Disability Rights Washington DOC assigns health services codes to every individual incarcerated in its system. These codes, known as PULHES or PULHES-DXTR codes, are meant to note the presence and severity of various health-related factors, such as medication delivery requirements, mobility limitations, developmental disability, and use of mental health services. The PULHES R code should reflect a person’s history of self-harm: R-0 is the default (no data), R-1 indicates there is no history of self-harm or suicide attempt in the past ten years, R-2 indicates that there is a history of self-harm or suicide attempt in the past ten years. 9 10 DOC reports that transfer delays have occurred due to Covid-19 restrictions. DOC reports that RTU admission/transfer process must remain extremely flexible to allow maximum benefit to incarcerated individuals and staff. 11 OCO Systemic Report: Mental Health Access & Services Page 9 Washington (DRW) also were invited and sent representatives. OCO was encouraged by the frank discussion that took place over the course of the two-day kickoff meeting in November 2019. Subcommittees continued to meet, and a second workgroup meeting occurred in February 2020. However, all subsequent meetings were canceled and tasks associated with the workgroup were put on hold due to the Covid-19 pandemic. VII. Individual Behavior Management Plans (IBMPs) Clear guidelines do not exist for the creation of IBMPs and IBMPs vary significantly in detail and individualization. 12 Individual Behavior Management Plans are one of a handful of tools that DOC may employ in an effort to support behavior modification for incarcerated individuals. IBMPs are typically created when mental health staff are aware that an individual is engaging in on-going, challenging behaviors that are associated with some underlying mental health condition. This tool has the potential to be extremely powerful: if successfully carried out, IBMPs can facilitate behavior change that is beneficial to the incarcerated individual, other incarcerated individuals, and DOC staff. Among these benefits are a less restrictive setting for the individual and a safer environment for other incarcerated individuals and staff. However, no policy exists that directs DOC on when, how, or for whom an IBMP should be created. OCO has observed that plans vary significantly from facility to facility. OCO has also observed that some plans focus on punitive responses to behaviors, including the use of restraints, rather than incentivizing positive behaviors. OCO believes that this is an underused, sometimes misused, tool that, when implemented correctly, has the potential to contribute significantly toward better conditions system-wide. VIII. Intensive Management Unit (IMU) Placement People with past and present mental health conditions frequently are assigned to segregated housing for extended periods of time. This practice goes against years of research that has shown that time spent in solitary confinement exacerbates mental health symptoms. Specific complaints relayed to OCO describe the impact of segregation exacerbating symptoms of mental health disorders, sometimes resulting in destructive or self-harming behaviors, often resulting in infractions and sanctions, causing time in solitary confinement to be repeatedly extended or increasingly harsh. DOC reports that a revised version of the IBMP protocol has been drafted that addresses many of these concerns. 12 OCO Systemic Report: Mental Health Access & Services Page 10 OCO has also observed that people who have been deemed unsuitable for Residential Treatment Units – often due to persistent disruptive behavior or failing to engage in treatment – have limited appropriate housing options. As a result, these individuals, often diagnosed with personality disorders (in contrast to mood disorders), are routinely placed in IMUs. OCO is concerned that individuals’ symptoms may be exacerbated once placed in segregation. For those people who do not experience psychiatric decompensation, the social and physical environment of IMU is not therapeutic, making it difficult to effectively receive and benefit from treatment. 13 IX. Americans with Disabilities Act (ADA) Accommodations: Individuals with psychiatric disabilities sometimes experience difficulty securing necessary modifications to programs, services, and activities via DOC’s accommodation request process. OCO has observed DOC’s difficulty bridging its ADA and mental health siloes in order to provide ADA-mandated accommodations to someone who has a mental health disability. OCO has observed instances in which FRMT records do not reflect multi-disciplinary collaboration with regard to accommodations. DOC’s response to OCO’s Persons with Disabilities report indicated a willingness to establish multi-disciplinary teams to handle these situations, but the progress of this work is unknown. Specific complaints relayed to OCO include: • • • An insufficient number of jobs for incarcerated people exist in some closed treatment areas. Some off-unit supervisors express disinterest in hiring and supporting someone with a mental health condition as an employee. In some cases, DOC required an individual to actively engage in some form of mental health treatment before agreeing to grant an accommodation related to the psychiatric disability. X. Support & Training for Staff DOC staff members may benefit from additional training to positively and effectively engage with individuals who have mental health conditions. Many of DOC reports that their collaborations with Amend and the Vera Institute of Justice have addressed these concerns, in part. DOC’s internal Restrictive Housing Workgroup continues to craft and implement related changes. 13 OCO Systemic Report: Mental Health Access & Services Page 11 the complaints received by OCO that relate to mental health allege some component of inappropriate or less than ideal staff conduct, such as: • • Individuals have reported instances in which custody staff in RTUs allegedly failed to act when an individual expressed self-harm or suicidal ideation. Individuals have reported instances in which some IMU staff members allegedly did not adequately or appropriately respond to people experiencing an increase in mental health symptoms and/or people in mental health crisis. XI. Special Populations14 Individuals who have been returned to prison from community custody or transferred to prison from jail often have unique needs that demand specialized focus from DOC staff. Individuals in this status (typically referred to as “violators”) frequently arrive having recently used substances and then are forced into rapid detox. Individuals who have been arrested and need mental health assessment and stabilization are often sent to prison for these services, where they are added to the already significant caseloads of DOC mental health providers. Additionally, when people in violator status have never been to prison before, department staff have no medical or mental health history that can inform treatment decisions. Even when a violator is returning to prison, that person’s health records are not readily available immediately upon return. XII. Administrative Concerns DOC can take additional steps to ensure access to ongoing, quality mental health care. OCO is unaware of any quality assurance and improvement processes that DOC has in place which include a specialized focus on mental health care. 15 OCO was informed that a Memorandum of Understanding between DOC and Washington’s Department of Social and Health Services (DSHS) regarding temporary transfers to a state psychiatric hospital has remained pending for many years. DOC Various stakeholders have relayed concerns to OCO regarding the minimal release planning conducted for individuals with mental health conditions. While OCO recognizes the tremendous importance of release planning for this population, we have not opened cases on the topic because we do not have jurisdiction over individuals outside of DOC’s physical custody. 14 OCO Systemic Report: Mental Health Access & Services Page 12 mental health providers have indicated to OCO that there are many individuals incarcerated in DOC who, these providers believe, are too ill to be housed in prison or require treatment that cannot be provided by DOC. Facilitating transfer to a state psychiatric hospital would at least provide the opportunity and appropriate setting for periodic patient stabilization when necessary. Recommendations I. Screening & Assessment Recommendation 1: DOC should review and revise the current mental health screening and assessment processes to: a. Achieve a more reasonable daily caseload that allows staff to perform a thorough review of the documents accompanying new intakes. b. Ensure that suitably confidential space exists where mental health staff are able to screen and assess individuals. c. Ensure that assessments are provided on a timely basis. II. Psychotherapy Recommendation 2: DOC should ensure that quality, timely mental health treatment services are available to anyone in DOC custody who demonstrates a clinical need for treatment. Efforts to address this may include increasing the number of qualified mental health providers available to provide short- and longterm mental health treatment services. 16 Recommendation 3: DOC should ensure maximum availability of group therapy. This could include prioritizing custody coverage of all necessary spaces proposed for use by mental health providers. Ideally, this could shift custody time to supporting individuals as they return to or sustain stability, rather than using custody time to respond to incidents stemming from mental health crises. Recommendation 4: DOC should meet the demand for additional mental wellness programs available to assist incarcerated people with addressing past trauma. This could include developing additional programs led by qualified DOC reports that it had prepared a request package before the pandemic that was submitted for legislative approval in the 2020-21 session. If approved in full, the proposal would have funded additional mental health staff positions, reducing mental health providers’ caseloads from approximately 90 patients to approximately 70 patients. 16 OCO Systemic Report: Mental Health Access & Services Page 13 individuals (staff and/or volunteers) and/or implementing evidence-based peer support programs. Recommendation 5: DOC should create better behavioral health linkages for individuals in work release. This could include re-creating a work release program with a special focus on supporting individuals with mental health needs. Recommendation 6: DOC should support race equity measures by ensuring that the demographics of mental health staff and contract providers reflect the racial and ethnic diversity of the incarcerated population. III. Medication Recommendation 7: DOC should ensure that prescribers are no longer discontinuing medications without first meeting with the patient to plan for this. Resolving this may include tracking data to ensure that this practice is no longer occurring. Recommendation 8: When grave disability is being considered for the basis of a referral for involuntary antipsychotic medications, DOC should provide the patient with objective indicators of self-care for the patient to demonstrate for some sustained period of time. IV. Disciplinary Process Recommendation 9: DOC should ensure that an individual’s mental health status is considered throughout the disciplinary process. Changes to ensure consideration of mental health status may include implementation of a unique policy or protocol to allow different handling of disciplinary cases for individuals who are assessed as S-3 or higher17, infracted while in an RTU or COA, or when the circumstances indicate a need for input from mental health staff in order to fairly determine guilt and sanctions. The PULHES S code is meant to reflect a person’s mental health service utilization. Any number greater than 1 (no identified mental health need) indicates that the person is on DOC’s mental health caseload. S codes 2, 3, 4, and 5 (most significant) reflect increasing mental health services use and needs. 17 OCO Systemic Report: Mental Health Access & Services Page 14 V. Self-Harm & Close Observation Areas 18 Recommendation 10: DOC should ensure all appropriate staff are aware of the need to update PULHES-DXTR R codes. Recommendation 11: DOC should ensure staff are adhering to the requirements of DOC 320.265 Close Observation Areas related to the creation of mental health safety plans prior to discharge from COA. Recommendation 12: DOC should ensure that suitably confidential space exists where mental health staff are able to meet with and assess individuals. Recommendation 13: DOC should ensure that approved transfers out of COA are prioritized. VI. RTUs Recommendation 14: DOC should develop a comprehensive RTU policy that addresses: a. objective criteria for admission; b. modified disciplinary system; c. modified classification system; d. pathway out of RTU, including objective criteria for discharge; e. mandatory specialized mental health training for RTU custody staff; and f. programming availability in RTU (to include programming support). VII. IBMPs Recommendation 15: DOC should develop a comprehensive IBMP policy, which may include: a. objective criteria for who should or must have an IBMP; b. guidelines for incentives that may be used; c. guidelines for safety responses that may be used, including whether/when use of restraints may be part of an IBMP; d. mandatory training for all mental health providers that addresses how to write an IBMP; e. mandatory training for any DOC custody staff who routinely work with individuals who have IBMPs; and DOC reports that the Chiefs of Psychology initiated in April 2021 an audit of all COA admissions. The audit will conclude in June 2021. 18 OCO Systemic Report: Mental Health Access & Services Page 15 f. routine audits of IBMPs by qualified headquarters staff. VIII. IMU Placement Recommendation 16: DOC should reduce the frequency of placement and the length of stay in any segregated housing, including A and B units of SOU, for individuals with serious mental health conditions. Recommendation 17: DOC should explore best practices for successfully housing and treating individuals with behavioral challenges, regardless of diagnosis, in a setting that is not IMU or other segregated housing. IX. ADA Accommodations Recommendation 18: DOC should continue to use multi-disciplinary teams to routinely address the need for accommodations that arise from individuals’ mental health disabilities. X. Support & Training for Staff Recommendation 19: In order to equip DOC correctional officers and other staff with the knowledge and skills needed to support individuals with mental health conditions, DOC should: a. Strive to facilitate culture change among staff in order to best support incarcerated individuals, the efforts of mental health staff, as well as goals associated with institutional safety. b. Set and communicate clear conduct and support expectations for all staff members who interact with individuals who have mental health conditions. c. Provide in-depth mental health awareness trainings to all DOC staff. It is critical that staff are able to recognize behaviors associated to mental health conditions before they become problematic for the individual, staff, and facility. d. Provide in-depth training on de-escalation techniques to all DOC staff. e. Provide specialized training on mental health conditions and basic behavior theory to all staff who work in RTUs and all staff assigned to COAs. These staff members must be better able to understand how an individual’s behavior may be impacted by a mental health condition. f. Provide specialized training on mental health conditions to hearing officers and Resolution Program coordinators. OCO Systemic Report: Mental Health Access & Services Page 16 g. Consider implementing additional training strategies and requirements as used by other jurisdictions, including Oregon DOC. 19 XI. Special Populations Recommendation 20: DOC should create policy or protocol language that specifically addresses the unique needs of individuals in violator status. XII. Administrative Concerns Recommendation 21: DOC should ensure implementation of internal quality assurance measures for mental health care. This may include: a. Conducting an overall mental health system assessment. b. Implementing routine peer-review of mental health records to ensure quality and consistency across the system. Recommendation 22: DOC should work with DSHS to set a clear pathway to allow DOC to temporarily transfer individuals in need of in-patient psychiatric care to Eastern or Western State Hospitals. 19 See OAR 291-048-0220. OCO Systemic Report: Mental Health Access & Services Page 17 STATE OF WASHINGTON DEPARTMENT OF CORRECTIONS P.O. Box 41100 • Olympia, Washington 98504-1100 July 29, 2021 Joanna Cams Office of Co!1'ections Ombuds 2700 Evergreen Parkway NW Olympia, WA 98505 Dear Ms. Cams: The Washington Department of Co!1'ections appreciates the opportunity to respond to the June 26, 2021 Office of Co!1'ections Ombuds (OCO) report 011 the ' Mental Health Access & Servic.es.' Recommendation Rec.01nmendation 1: DOC should review and revise the ctment mental health screening and assessment processes to: a. Achieve a more reasonable daily caseload that allows staff to perfom1 a thorough review of the documents accompanying new intakes. b. Ensure that suitably confidential space exists where mental health staff are able to screen and assess individuals. C. Ensure that assessments are provided on a timely basis. Response The department is preparing decisions packages for the 2022 supplemental budget to request two additional psychology positions and capital funds to create a more effective in take/reception process. Recommendation 2: DOC should ensure that quality, timely mental health treatment services are available to anyone in DOC custody who demonstrates a clinical need for treatment. Efforts to address this may include increasing the number of qualified mental health providers available to provide short- and long- The department provides in the DOC health plan mental health assessment, medication and treatment se1v ices: h!ffis://www.doc.wa.gov/docs/publications/600HAO0l.pdf Staff p1io1itize treatment, to include individual and group therapy, psychiatii c medica tion, and case management services, based on clinical "Working Together for SAFER Communities" OCO Systemic Report: Mental Health Access & Services Page 18 Joanna Cams July 29, 2021 Page 2 tenn mental health treatment se1vices. Recommendation 3: DOC should ensure maximum availability of group therapy. This could include prioritizing custody coverage of all necessa1y spaces proposed for use by mental health providers. Ideally, this could shift custody time to supporting individuals as they return to or sustain stability, rather than using custody time to respond to incidents stemming from menta l health crises. assessment and evaluation. Individuals request se1vices via kite and department staff are trained to identify early indicators of mental health concerns and refer identified individuals for a mental health assessment. Individualized treatment is provided based on clinical assessment. The department routinely reviews its distribution of staffing resources to make sure positions are located where the greatest patient needs exist. The department is preparing a decision package to increase the number of mental health providers at key locations with the intent to provide mental health se1vices for more individuals. Many facilities continue to experience COVID-19 as a banierto increasing the use of group therapy. The physical space available to accommodate groups with appropriate co!1'ectional supe1vision is a significant banier to providing more group therapy. Leadership for psychology and health se1vices at each facility have been asked to evaluate the physical space available at each co1Tectional facility and identify potential space available to hold treatment groups. The health services managers will then work with p1ison administrators to develop implementation plans for utilization of those spaces. If additional resources are needed to create access to space this work will help to infonn decision packages in ctl!1'ent and future years. The assessment of space is estimated to be completed in September 30, 2021. Recommendation 4: DOC should meet the demand for additional mental wellness programs available The department is contracted with Amend at the University of California-San Francisco. The p1ima1y focus of this work is to identify and "Working Together for SAFER Communities" OCO Systemic Report: Mental Health Access & Services Page 19 Joanna Cams July 29, 2021 Page 3 to assist incarcerated people with addressing past trauma. This could include developing additional programs led by qualified individuals (staff and/or volunteers) and/or implementing evidence-based peer support programs. incorporate a co1Tectional culture with a public health-oriented mission. The work is focused on creating a healthier prison population, staff and communities. One of the goals of the partnership is the improvement of the health and wellbeing of the incarcerated and avoidance of re-traumatization. A comprehensive list of the therapy and support programs available through the department can be found at https://w,vw.doc.wa.gov/co1Tections/programs/d escriptions.htm - therapy-support. In collaboration with the department's con-ectional program administrator and family & volunteer services manager, there are a series of steps planned to re-introduce these programs as the state 's con-ectional facilities begin reopening following COVID-19. Below are two importan t examples of popular and effective "peer-based" programs utilized in support of thos e in the department's custody and care: Yoga Behind Bars (YBB) is a ve1y popular evidence-based activity led by trained incarcerated individuals. There are plans to expand the YBB program across more facilities. There is a trauma-based component of the YBB program, which will be included in the training of new leaders and roll-out of the program across most con-ectional facilities. Alcoholic Anonymous/Narcotics Anonymous (AA/NA) groups are volunteer-led groups offered at most, if not all, facilities. Availability is dependent on volunteers though this has historically not been a challenge. The department identified funding available through the Incarcerated Individual Bettennent Fund (IIBF) that will be used to research, develop and introduce a pilot program to focus on wellness within the next 12 months. " Working Together for SAFER Communities" OCO Systemic Report: Mental Health Access & Services Page 20 Joanna Cams July 29, 2021 Page 4 Recommendation 5: DOC should create better behavioral health linkages for individuals in work release. This could include recreating a work release program with a special focus on supporting individuals with mental health needs. The department has developed a continuity of care document for use with the Health Care Authority (HCA) and managed care providers and is slated for implementation by November 30, 2021 . This will be the fotmdation for a similar plan for those people transitioning from a state con-ectional facility to work release. The work release programs have individualized plans, which may include exclusive focus on treatment. The department will continue efforts across organizational divisions (Prisons, Reentiy, Health Se1vices, Community Co1Tections) to develop and implement a plan for greater collaboration to ensure treatment needs are met in the community. Recommendation 6: DOC should support race equity measures by ensuring that the demographics of mental health staff and contract providers reflect the racial and ethnic diversity of the incarcerated population. The Mental Health Leadership Team will continue to consult with Equity and Inclusion Administrator Dr. Ad1ian Thompson and the health se1v ices staffrecrnitment team about ways in which to improve the racial and ethnic diversity of mental health staff. These efforts will include more intentional recrnitment strategies such as career postings with professional groups for people of color. Plans will be developed in collaboration with Dr. Thompson to improve retention of staff. This may include mentoring opportunities as well as training in cultural competence. Recommendation 7: DOC should ensure that prescribers are no longer discontinuing medications without first meeting with the patient to plan for this. Resolving this may include tracking data to ensure that this practice is no longer occuning. A memo was sent to all psychiatric prescribers by the director of mental health and the chief of psychiatry in July 2020, with a follow-up in June 2021. The memo strictly prohibited the discontinuation of medications without having assessed the patient and discussed it with them. The chiefs of psychology, the chief of psychiat1y and health services managers are expected to use vigilan t supe1v ision to identify if this occurs, even if a patient does not report a concem. This will be monitored through filed izrievances and accom1tability "Working Together for SAFER Communities" OCO Systemic Report: Mental Health Access & Services Page 21 Joanna Cams July 29, 2021 Page 5 checks with health care providers, if such prac:tices are detennined to have resrnfaced, a more vigorous approach will be considered. Recommendation 8: When grave disability is being considered for the basis of a refeffal for involuntaiy a ntipsychotic medications, DOC s hould provide the patient with objective indicators of self-care for the patient to demonstrate for some s ustained period of time. The self-management of psychiatric symptoms fo1m (Attachment A) was developed for use when considering involunta1y antipsychotic medications. An official agency fonn is developed and will be published by July 30, 2021 . The fonn identifies the expected behaviors indicative of adequate self-care. The fo1m gives the patient up to 30 days (the timeframe can be varied based on patient need, health and safety) to improve prior to a refeffal for involuntaiy medications. Training of staff will occm by July 30, 2021. Recommendation 9: DOC should ensure that an individual's mental health status is considered throughout the disciplimuy process. Changes to ensure consideration of mental health s tatus may include implementation of a tmique policy or protocol to allow different handling of disciplinaiy cases for individuals who are assessed as S-3 or higher, infracted while in an RTU or COA, or when the circumstances indicate a need for in put from mental health staff in o rder to fairly detennine guilt and s anction In March 2021, the department began to pilot a new disciplina1y process at Washington Co!l'ections Center for Women (WCCW) and Monroe Con-ectional Complex-Special Offender Unit for those people with a serious mental illness. The pilot includes a review of serious infractions by a person's prima1y therapist. The review is used to detennine whether fi.mctional limitations contributed to the infracted behavior and whether the person has the mental status to participate in the infraction hearing. If either of thes e situations is found, the infraction will be dismissed. When the infraction is dismissed, the treatment team is responsible for the development of an inte1v ention plan to assist in the reduction or elimination of the concerning behavior. If the infraction does result in a hearing and the infraction is upheld, the treatment team will recommend a modified sanction designed to assis t the person in the reduction or elimination of the behavior. These individuals are not subject to the traditional sanctions used in the disciplina1y process. The pilot is modeled after a program in the Oree:.o n Department of "Working Together for SAFER Communities" OCO Systemic Report: Mental Health Access & Services Page 22 Joanna Cams July 29, 2021 Page 6 Coffections and is scheduled to conclude at the end of September 2021 . After the conclusion of the pilot, the procedure (Attachment B) will be reviewed and adjusted as needed and is expected to roll out more broadly in the first quarter of 2022. Recommendation 10: DOC should ensure all appropriate staff are aware of the need to update PULHESDXTR R codes. Refresher training was provided on May 20, 2021 to all psychologist 4 staff to review the criteria for establishing R codes and the expectations for making necessaiy updates to those codes. These staff have been directed to reinforce with their staff the importance of reliable reporting of these codes. The chiefs of psychology will monitor the completion of the training and ensure all staff have been reminded of the importance of reliable coding by July 31, 2021. Recommendation 11 : DOC should ensure staff are adhering to the requirements of DOC 320.265 Close Obse1v ation Areas related to the creation of menta l health safety plans prior to discharge from COA. Active monitoring of all close observation area (COA) admissions and discharges by the chiefs of psychology began in March 2021. The monitoring ensures that per protocol and policy, discharge suicide risk assessment (SRA) evaluations are conducted along with safety plans before a person is released from the COA. The monitoring includes quarterly audits for COA documentation by each chief of psychology. Recommendation 12: DOC should ensure that suitably confidential space exists where mental health staff are able to meet with and assess individuals The chiefs of psychology assessed the physical plant of each COA location to identify the confidential space adjacent to the COA w here inte1views and evaluations may occm. The assessments of inte1v iew spaces were completed as of June 30, 2021 . Health se1v ices managers and prison administrators will be notified of any areas tha t do not have confidential inte1v iew spaces and will be asked to collaborate on how this can be addressed. Recommendation 13 : DOC should ensure that approved transfers out of COA are prioritized. Transportation agrees that transfers will occur with four or less people, when needed, to move a person out of the COA. Headquarters-based classification staff will be monitoring the "Working Together for SAFER Communities" OCO Systemic Report: Mental Health Access & Services Page 23 Joanna Cams July 29, 2021 Page 7 timeliness of the classification process for these individuals. Mental health leadership will continue to work closely with classification and transportation staff to priodtize individuals to minimize length of stay in COAs. Recommendation 14: DOC should develop a comprehensive RTU policy that addresses: a. objective criteria for admission; b. modified disciplina1y system; C. modified classification system; d. pathway out of RTU, including objective criteria for discharge; e. mandato1y specialized mental health training for RTU custody staff; and f. programming availability in RTU (to include programming support). The residential treatment unit (RTU) workgroup is expected to begin meeting by the end of August 2021 . The workgroup includes health services, prisons and classification staff along with representation from OCO and Disability Rights Washington (DRW). The charter of the workgroup includes the development of policy to support the RTU. The policy will address the process and general criteria for admission and discharge from RTU level of care, and training for staff working in RTUs. The modification of the disciplinaiy process to accommodate those individuals with serious mental illness is ctmently being piloted as discussed above and includes modified sanctions and behavioral approaches designed to support those with mental health conditions. A modification of the classification system for those people placed in residential treatment units will be discussed for changes to the classification policy. Efforts to identify and implement additional programming opportm1ities continue in coordination with the Reent1y Division and local community-based organizations. Recommendation 15 : DOC should develop a comprehensive IBMP policy, which may include: a. objective criteria for who should or must have an IBMP; guidelines for incentives that b. maybe used; c. guidelines for safetv The Managing Challenging Mental Health Patient Protocol, which directs the development and implementation of individual behavior management plans (IBMP), was updated to improve the multi-disciplinaiy approach to the IBMP process as well as insure greater utilization of incentivizing prosocial behaviors over ending negative behaviors. (Attachment C). The department will develop euidelines for "Working Together for SAFER Communities" OCO Systemic Report: Mental Health Access & Services Page 24 Joanna Cams July 29, 2021 Page 8 responses that may be used, including whether/when use of restraints may be part of an IBMP; d. mandato1y training for all mental health providers that addresses how to write an IBMP; e. mandato1y training for any DOC custody staff who routinely work with individuals who have IBMPs; and f. routine audits of IBMPs by qualified headqua11ers staff. Recommendation 16: DOC should reduce the frequency of placement and the length of stay in any segregated housing, including A and B units of SOU, for individuals with serious mental health conditions. incentives to be used to improve standardization across facilities. It is key however, that flexibility remains so that the incentives included in the IBMP is as individualized as possible. The updated protocol calls for IBMPs continued beyond six months to be reviewed by a chief of psychology to ensure the quality and efficacy of the plans developed and implemented. The psychologist 4s, who are most frequently invo!Yed in developing IBMPs, were trained on the updated protocol on June 3, 2021 . Training for other staff involved with the implementation ofIBMPs, to include coffectional officers, will be developed by Oct. 1, 2021 and implemented by Janua1y 2022. Througl1 work with the Vera Institute of Justice and Amend, the depanment has progressively addressed both the frequency and length of stay in restrictive housing. The department's use of restrictive housing has consistently declined since 2012, particularly for those with serious mental health concerns. Since 2012, the administrative segregation population has been reduced by a third (Over 570 in 2012, 420 June of 2021 ). There has been a:'\:'\ percent <lecrea.c:e in the median length of stay in maximum custody and a 45 percent reduction in selfhann/suicide attempts in restrictive housing. The department also reviewed the number of extensions for investigations past 30 days and has developed strategies for a more rigorous consideration process to be used when considering approval for those extensions . The department has increased its scrutiny of those who have extensions granted to farther reduce the length of stay in restricted settings were 11JJJJW]Jrialt::. By policy, the department has stopped the use of assigning disciplina1y segregation as a sanction and instead focus on sanctions designed to disincentivize behaviors of concern. Work is being done to pilot projects like "Working Together for SAFER Communities" OCO Systemic Report: Mental Health Access & Services Page 25 Joanna Cams July 29, 2021 Page 9 transfer pods and transition pods to limit restrictive housing and place incarcerated individuals in the least restrictive environment given their circumstances. Recommendation 17: DOC should explore best practices for successfully housing and trea ting individuals with behavioral challenges, regardless of diagnosis, in a setting that is not !MU or other segregated housing. As the department expands its continuum of care by developing strategies for intensive outpatient treatment (i.e. more frequent therapeutic inte1ven tions), it is expected that some of these individuals' treatment needs will be met in a general population and reduce the frequency of placement in restrictive housing. I.nfonnation and documentation gathered from programs in the New York and Massachusetts con-ectional systems are being reviewed and considered to detem1ine if similar programs may be a good fit for the department and those in our facilities . These programs include small units (40-100 beds), an emphasis on incentivizing behavior and the use of dialectical behavior and cognitive behavioral treatment approaches. The department this includes an assessment of ctmently available physical plant and operational resources to detennine feasibility for implementing a similarly designed program. Recommendation 18: DOC should continue to use multi-discipl!ina1y teams to routinely address the need for accommodations that aris e from individuals' mental health disabilities. The department will continue to use multidisciplina1y teams to routinely address the need for accommodations that arise from an individual's mental health disabilities. Recommendation 19: In order to In collaboration with the training and equip DOC co!1'ectiona.l officers and development unit (TDU): other staff with the knowledge and skills needed to support individuals with me11tal health conditions, DOC should: a. Strive to facilitate culture change among staff in order a. Culture change is a constant goal of the agency and is communicated via the mission, vision and values training cun-ently assigned to new employee orientation (NEO) for all new staff and annual in-se1vice (AIS) and the leadership values course for supe1visors. " Working Together for SAFER Communities" OCO Systemic Report: Mental Health Access & Services Page 26 Joanna Cams July 29, 2021 Page 10 b. C. d. e. f. g. to best support incarcerated individuals, the efforts of mental health staff, as well as goals associated with institutional safety. Set and co111111unicate clear conduct and support expectations for all staff members who interact with individuals who have mental health conditions. Provide in-depth mental health awareness trainings to all DOC staff. It is critical that staff are able to recognize behaviors associated to mental health conditions before they become problematic for the individual, staff, and facility. Provide in-depth training on de-escalation techniques to all DOC staff. Provide specialized training on mental health conditions and basic behavior theo1y to all staff who work in RTUs and all staff assigned to COAs. These staff members must be better able to tmderstand how an individual's behavior may be impacted by a mental health condition. Provide specialized training on mental health conditions to hearing officers and Resolution Program coordinators. Consider implementing additional training strategies and requirements as used by other jmisdictions, including Oregon DOC. b. Staff working in specific areas where individuals are known to have a mental health concem, such as an RTU, specific training objectives are addressed through the RTU workgroup. Because a person's functioning is impacted by a mental illness, they may not clearly express their needs and for this reason, it is recommended that a "universal precautions" approach be used and respond by engaging the person and assisting them with identifying their concerns or making refe1nls. Staff are expected to address all people with respect and individually. C. Training specific to individuals experiencing mental health symptoms is provided to all staff who attend both con11mmity co1Tections officer academy (CCOA) and co1Tectional worker core (CWC). The training is instructed by mental health professionals and is two hours in length. In-depth de-escalation techniques are d. taught to all staff drning both academies (CCOA and CWC). In addition, it is part of the CCOA AIS. For new employee orientation (NEO), the training is an eight-hour course. The employees attending ewe receive 12 hours of training. Employees receive six hours of initial training in CCOA. e. & f. More specific training can be developed and provided to people in specialized job classes. Such training would require resomces to develop appropriate cu1Ticula, instrnct courses and establish the training as a priority for the agency. A proposal for what would be required for these reco1mnendations will be prepared for presentation to the department's executive leadership by September 30, 2021. g , The department will connect with its "Working Together for SAFER Communities" OCO Systemic Report: Mental Health Access & Services Page 27 Joanna Cams July 29, 2021 Page 11 counterparts in Oregon and other jurisdictions to leam more about tlleir programming and detennine if there are components that can assist with enhancing training. Recommendation 20: DOC should create policy or protocol language that specifically addresses the unique needs of individuals in violator status. The department recognizes the unique healthcare needs of those in violator status. To further adapt the screening, assessment and treatment process for the unique population, a workgroup will be fonned to address the need to develop policy and protocol to address the population. The initial charter of the workgroup has been drafted and participan ts identified (Attachment D). The workgroup is targeted to begin meeting by August 15, 2021. The department is also reviewing options for both contracting and resource requests that may be part of decision packages this year and in the future to support targeted resources within state con-ectional facilities for those held on a community violation and increase the use of community jail beds. Recommendation 21 : DOC should ensure implementation of internal quality assurance measures for mental health care. This may include: a. Conducting an overall mental health system assessment. b. Implementing routine peerreview of mental health records to ensure quality and consistency across the system. The mental health leadership at the department developed an audit tool that provides an indepth assessment of the quality of mental health services provided to individuals in the department's custody (Attachment E). The tool is used as a component of clinical supe1v ision (peer-to-peer) as well as in the biannual operational inspections conducted at each facility. All mental health staff meet with their supe1visors on a regular basis, the frequency of which is not less than monthly. Chart documentation is reviewed and evaluated according to the standards in the audit tool. The outcomes of the chart audits provide guidance for the clinical staff to improve their work, as documented on superviso1y conference fo1ms. This model of clinical supe1v ision is consistent with industry standards. "Working Together for SAFER Communities" OCO Systemic Report: Mental Health Access & Services Page 28 Joanna Cams July 29, 2021 Page 12 In addition to these audits, the biannual operational inspections provide a facility-wide assessment of the quality of menta l health services and identify any systemic concerns at each location. Action plans developed from the outcomes of the operational inspections address any concerns in the quality of care provided. Reconunendation 22: DOC should work with DSHS to set a clear pathway to allow DOC to temporarily transfer individuals in need of inpatient psychiatric care to Eastern or Westem State Hospitals. The department recognizes access to inpatient psychiatric care for the most severely mentally ill population can be an important tool. A statuto1y mechanism exists that authorize, a transfer between the Department of Co!1'ections to an inpatient institution that cares for the mentally ill. Court decisions also require certain procedural safeguards prior to such transfers. Additionally, any transfers would need to be accomplished in a manner that also allow, the Department of Social and Health Services (DSHS) to accomplish its broader mission. The department has explored the possibility of a MOU with DSHS, but it has yet to find a workable MOU that meets these goals. The department can continue to fmther explore such an MOU. The department would like to emphasize its continued committed to providing care to those individuals w ho remain in department custody and any process that would be developed to transfer someone to an inpatient facility would only be considered to provide care once all care options within the department are exhausted. The infonnation provided in the mental health access & se1vices systemic report by the Office of Co!1'ections Ombuds was useful to ensm·e the Department of Co!1'ections is designed and managed to provide safety for the persons in its custody. We also appreciate your team's understanding of the unique processes across the co!1'ectional system and the addition otpolicies and procedures, as well as additional resource requests, being put in place to address them. We are working proactively to continuously improve quality assurance standards tlu·oughout the department. "Working Together for SAFER Communities" OCO Systemic Report: Mental Health Access & Services Page 29 Joanna Cams July 29, 2021 Page 13 Moving fo1ward, the Washington Department of Con-ections will continue to collaborate w ith the Office of the Con-ections Ombuds to strengthen procedures and practices that positive impact individuals' health, safety and welfare. Sincerely, ~ ~ """" Policy Washington Department of Con-ections SM:kr cc : Che1y l Stran ge, Secreta1y Sean Mmphy, Deputy Secreta1y Julie Martin, Chief of Staff Jeremy Barclay, Director of Engagem ent and Outreach Attachment A: • Self-Management of Psychiatiic Symptoms Attachment B: • SMI Hearin gs MEMO & SMI Heatings m emo process (attached as 17-089) Attachment C : • Managing Challenging Mental Health Patients Protocol (IBMP) • 13-069 IBMP • 13-595 MH Functional Assessment Attachment D: • Project Charter Attachment E: • Monthly supervision score card • Operational Inspection Audit Preparation - MH Sections "Working Together for SAFER Communities" **The full DOC response with attachments can be found on the OCO website. OCO Systemic Report: Mental Health Access & Services Page 30