Emory CHIC, Coronavirus and the Correctional Facility, 2020
Download original document:

Document text

Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
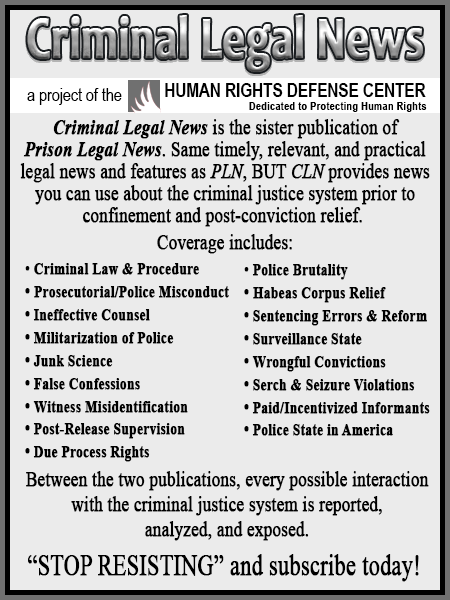
Coronavirus COVID-19 and the Correctional Facility For the Correctional Healthcare Worker Anne C. Spaulding MD MPH March 9, 2020 Emory Center for the Health of Incarcerated Persons Aspauld@emory.edu Development of these slides was supported under cooperative agreement, the Centers for Disease Control and Prevention’s (CDC’s) Collaboration with Academia to Strengthen Public Health Workforce Capacity (grant no. 3 U36 OE000002-04 S05) funded by CDC, Office of Public Health Preparedness and Response, through the Association of Schools and Programs of Public Health (ASPPH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of CDC, the Department of Health and Human Services, or ASPPH. Please do not alter content without contacting author. Outline • COVID-19 Overview for a Congregate Environment • • • • • Spread Prevention Symptoms & Diagnosis Treatment Adverse Outcomes • Implications for Correctional Healthcare • Overview • Correctional Facility Case Examples • Coordination • A Cautionary Tale COVID-19 Overview: Spread • COVID-19 is a viral disease • The virus’ official name is “SARS-CoV-2”; COVID-19 is the name of the disease • Transmission • • • • The virus is thought to spread mainly from person-to-person. Between people who are in close contact with one another (within about 6 feet) Via respiratory droplets produced when an infected person coughs or sneezes. Droplets can land in mouths or noses of people nearby or possibly be inhaled into lungs. • May spread from inanimate objects that have virus on them, but this is not the main way it spreads. • People are thought to be most contagious when they are the sickest. • Some spread might be possible before people show symptoms, but this is not the main way it spreads. COVID-19 Overview: Spread • COVID-19 is a viral disease • The virus’ official name is “SARS-CoV-2”; COVID-19 is the name of the disease • Transmission • • • • The virus is thought to spread mainly from person-to-person. Between people who are in close contact with one another (within about 6 feet) Via respiratory droplets produced when an infected person coughs or sneezes. Droplets can land in mouths or noses of people nearby or possibly be inhaled into lungs. • May spread from inanimate objects that have virus on them, but this is not the main way it spreads. • People are thought to be most contagious when they are the sickest. • Some spread might be possible before people show symptoms, but this is not the main way it spreads. COVID-19 Overview: Spread • The first cases were in the Hubei province of China. • It has now spread to many countries. • As of March 2020, some areas of the US have local transmission. • Keep up with your state and local health department to learn what’s happening where your correctional facility is located. Persons entering correctional facilities can have infections either Because of travel from, or through, a highly prevalent region, OR From acquisition of the infection close to home… If it’s spreading in your community, it’s likely to show up in your local jail or prison. COVID-19 Overview: Prevention Avoid close contact with people who are sick. Avoid touching your eyes, nose, and mouth. Cover your cough or sneeze with a tissue, then throw the tissue in the trash. Wash your hands with soap and water frequently. • Wash for 20 seconds—as long as it takes to sing the Happy Birthday song. • Clean and disinfect frequently touched objects and surfaces using a hospital-grade disinfectant. • Follow CDC’s recommendations for using a facemask, and isolation of infected persons. • • • • • Correctional staff should stay off from work if they feel sick. Have a cough, fever and/or shortness of breath? Stay home. If illness becomes worse, seek medical care; call ahead before you go! This slide can be printed out and used as a hand out for staff Health Alert Signage for the Health Services Unit—same as used for flu. Feel free to copy in color or black and white. Adapted from: https://www.bop .gov/resources/p dfs/seasonal_infl uenza_guidance. pdf Overview: Symptoms & Diagnosis • Many people are asymptomatic or only have mild symptoms. • Can appear soon (~ 2 days) or long (~2 weeks) after exposure. • Or sometime between “soon” and “long after”! • Some common symptoms: fever, cough, shortness of breath. • Which sounds an awful lot like the flu… Tip: To prevent influenza, and • possible unnecessary evaluation for COVID-19: use your flu vaccine stock now! See CDC.gov for up-to-date signage you can copy Overview: Symptoms & Diagnosis To review, the common symptoms are : 1) fever, 2) cough, and 3) shortness of breath. Diagnostic guidelines, best tests are evolving, so check your local and state health department for latest updates. Also: go to CDC.gov 1. CHECK where patient has been within 14 days of the onset of symptoms— -- Any place on current list of areas where there is local transmission?? 2. ASK about contact with an infected person. 3. ASSESS Symptoms—especially worrisome if 2 or more of the above symptoms. IF APPROPRIATE EXPOSURE HISTORY & SYMPTOMS: Put a simple surgical face mask on patient. Place them in a separate, closed room and shut the door. Ideally, use an airborne infection isolation room (AIIR) with neg. pressure. Healthcare and custody staff : wear personal protective equipment in room N-95masks/gowns/gloves, etc. Assess stability of patient—in respiratory distress needing hospital transfer? Or do you want to test them on site? Call your local health department for help. COVID-19, the new type of coronavirus For those not needing hospital transfer: • Treatment • • • • • Rest Drink fluids to prevent dehydration Take medicine to reduce fever (for example, acetaminophen) Research is ongoing on the use of already-developed medications Health care staff should be notified if patient worse symptoms develop, such as difficulty breathing. • Vaccination • There is no vaccine for COVID-19 as of early March 2020, but scientists around the world are actively working on a vaccine. This slide can be printed out and used as a hand out for patients. COVID-19 Complications Overview • Anyone can have a coronavirus infection that can become serious or be fatal. • Serious disease and death are most common in older persons and/or those with underlying medical conditions • Think of your patients in chronic care clinics, your pregnant patients and how you will keep them safe from disease. (See CDC website for guidance for particular groups, such as pregnant women.) Implications for Correctional Health Staff Are correctional facility populations at risk? Yes. 1. Healthcare staff should be aware of ongoing updates to clinical guidelines. 2. Share with your local health department the role of your facility in prevention, identification, and management of infectious disease. Remind them that you are in their territory. • Just because you have a healthcare staff… (which may be hired via a private vendor) …doesn’t mean that the health department should not consider how the presence of a jail and prison, and movement of citizens in and out of the facility, impacts the health of the public. 3. Work with your facility on planning now: where to cohort persons (placing persons diagnosed with coronavirus together, but at a distance from folks who are well) if many people are getting sick at the same time. Health Services: Check with your local health department and https://www.cdc.gov/coronavirus/ website as needed for latest guidelines on: 1. How to isolate persons—when is negative pressure room indicated? 2. How long to quarantine those who are exposed, those who are infected? 3. What personal protective equipment is needed, and for whom: N95 or surgical mask, eye shield, gloves, gowns? 4. How to handle those exposed to a case of COVID-19, especially after first test is negative: when to repeat before infection can be ruled out? 5. When can isolation be lifted? Implications for Correctional Custody Staff Are people who live and work in correctional facilities at risk? Yes. • Jurisdictions need to understand that incarceration of persons defying quarantine orders could lead to exponential increases in jail cases and cases in the community. • Measures other than detention should be considered, such as athome electronic monitoring. • Custody should plan on future absenteeism of ill correctional officers. • Supply chains (medicines, food, etc.) may become disrupted. • Consider alternatives to incarceration, in order to keep stock population down (diversionary courts, community corrections) . • If COVID-19 is in your jurisdiction, consider restriction of movement in and out (visitors, non-essential vendors, tours). Implications for Correctional Healthcare: A Florida Jail Case Example with Zika: PLAN now, before the epidemic reaches your jurisdiction 1. A protocol for the jail was developed with the help of local health department. 2. When a symptomatic entrant to the jail was confirmed with Zika infection, the Florida jail maintained close relationship with the local health department. Call your local health department now, even if the epidemic has not yet hit your town, to make sure that correctional health services are being considered in regional planning… Make sure they have your contact info Other Issues for Correctional Healthcare • Think of your supply chain for medications and medical supplies: realize that a continued epidemic may disrupt distribution of goods. Consider making sure your stocks are full, but don’t hoard. • Make sure persons confined in your facility have access to soap for hand washing; tissue for nasal discharge, etc. • Consider what will happen if health care workers are themselves sick and need to stay home, or if they are at home caring for others. • Prepare for absenteeism, and discourage “presentism”: when sick staff members insist on coming to work, and possibly infecting your patients. Implications for Correctional Healthcare: Two Cautionary Tales • Prisons and jails are enclosed environments, where individuals dwell in close proximity. Incarcerated persons sleep in close quarters, eat together, recreate in small spaces. Staff are close by. Both those incarcerated and those who watch over them are at risk for airborne infections. • A prison and jail is a self-contained environment. Implications for Correctional Healthcare: Two Cautionary Tales • Cautionary tale #2: Hundreds of cases diagnosed in Chinese prisons. Photo: S. China Post, from Weibo Photo: Fox News • Prisons and jails are enclosed environments, where individuals dwell in close proximity. Incarcerated persons sleep in close quarters, eat together, recreate in small spaces. Staff are close by. Both those incarcerated and those who watch over them are at risk for airborne infections. • A prison and jail is a self-contained environment. • Some make an analogy with a cruise ship. • Cautionary tale #1: think of the spread of COVID-19 on the Diamond Princess Cruise Ship, January 2020. Resources: • https://www.cdc.gov/coronavirus/2019-ncov/index.html Many correctional systems have developed pandemic flu plans. These plans can be readily adapted to COVID-19 and readapted as we learn more about this new pathogen, e.g., incubation period, transmission, and morbidity factors. The BOP plan is available online: • https://www.bop.gov/resources/pdfs/seasonal_influenza_guidance.pdf • Questions? Aspauld@emory.edu • Emory Center for the Health of Incarcerated Persons, Atlanta GA Acknowledgments: I am grateful for constructive criticism from Allison Chamberlain, Newton Kendig, Ank Nijhawan, Dianne Rechtine, Marc Stern, and countless colleagues who are federal/state employees. 3/9/2020