Analysis of 2019 Suicide Deaths in Washington DOC (1)
Download original document:
Document text
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
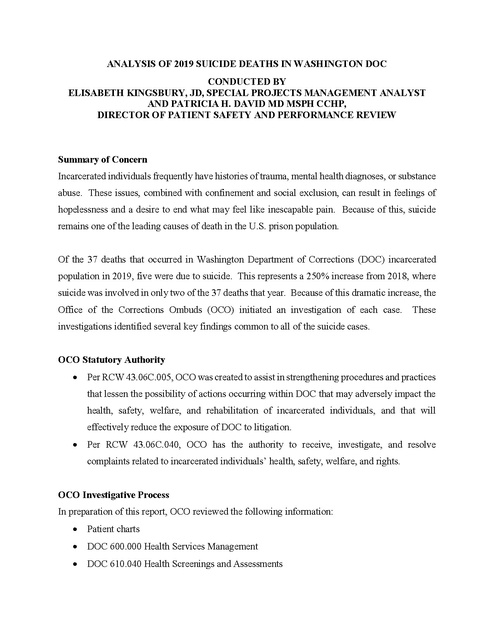
ANALYSIS OF 2019 SUICIDE DEATHS IN WASHINGTON DOC CONDUCTED BY ELISABETH KINGSBURY, JD, SPECIAL PROJECTS MANAGEMENT ANALYST AND PATRICIA H. DAVID MD MSPH CCHP, DIRECTOR OF PATIENT SAFETY AND PERFORMANCE REVIEW Summary of Concern Incarcerated individuals frequently have histories of trauma, mental health diagnoses, or substance abuse. These issues, combined with confinement and social exclusion, can result in feelings of hopelessness and a desire to end what may feel like inescapable pain. Because of this, suicide remains one of the leading causes of death in the U.S. prison population. Of the 37 deaths that occurred in Washington Department of Corrections (DOC) incarcerated population in 2019, five were due to suicide. This represents a 250% increase from 2018, where suicide was involved in only two of the 37 deaths that year. Because of this dramatic increase, the Office of the Corrections Ombuds (OCO) initiated an investigation of each case. These investigations identified several key findings common to all of the suicide cases. OCO Statutory Authority • Per RCW 43.06C.005, OCO was created to assist in strengthening procedures and practices that lessen the possibility of actions occurring within DOC that may adversely impact the health, safety, welfare, and rehabilitation of incarcerated individuals, and that will effectively reduce the exposure of DOC to litigation. • Per RCW 43.06C.040, OCO has the authority to receive, investigate, and resolve complaints related to incarcerated individuals’ health, safety, welfare, and rights. OCO Investigative Process In preparation of this report, OCO reviewed the following information: • Patient charts • DOC 600.000 Health Services Management • DOC 610.040 Health Screenings and Assessments • DOC 610.650 Outpatient Services • DOC 630.500 Mental Health Services • DOC 850.015 Staff Counseling and Employee Assistance • DOC 890.620 Emergency Medical Treatment, • DOC Suicide Risk Assessment Protocol, and • Offender Health Plan. In addition, OCO interviewed DOC staff, and reviewed DOC internal correspondence and incident reports. Case Overview Patient A was 38 years old when he arrived at DOC under violator status on March 6, 2019. At intake, he reported to DOC staff that he had attempted suicide twice previously, with the most recent occurring within the last two months. The following day, he informed his correctional counselor that he attempted suicide the night before, and voiced his ongoing desire to kill himself. This critical information was not clearly communicated to the mental health staff assigned to him. Furthermore, the mental health staff failed to properly evaluate Patient A, opting to converse with him at cell front rather than moving him to a private interview room to perform a thorough evaluation and Suicide Risk Assessment. He complained of right eye pain on March 8, 2019 and was taken to the emergency department where tests did not reveal a clear source of his pain. On March 9, 2019 medical staff noticed a change in Patient A’s baseline behavior but did not notify others. Throughout the day, custody staff, medical staff, and other incarcerated individuals observed Patient A screaming out in pain and asking for help. Patient A pushed his emergency call button multiple times throughout the day, calling for medical support. Because he had already been evaluated in the ER, the RN on duty believed that there was nothing else that could be done for Patient A, and attempted to dissuade him from using the emergency call button by threatening him with a $4.00 copay if he continued. Finally, Patient A pulled the emergency cord out of the wall, initiating both a light and a continuous alarm. The CNA on duty approached a correctional officer regarding the alarm, but was told it would be handled later since it was shift change. The CNA silenced the alarm. Seventeen minutes later, staff observed Patient a hanging from that emergency cord. DOC staff subsequently initiated the facility emergency medical response, and Patient A was taken to the hospital. After 11 days on a ventilator, Patient A’s family made the decision to remove him from life support and he passed away. His death was ruled a suicide. OCO Findings: Delay in access to care; failure to recognize, evaluate, and/or manage “red flags;” failure of communication between staff; failure of communication with incarcerated individual; failure to follow DOC policies Patient B was remanded to DOC custody on June 6, 2019. He was housed at Washington Corrections Center (WCC) until August 21, 2019, at which time he was transferred to WSP. Upon arrival at WSP he was infracted for allegedly attempting to introduce contraband, in the form of drugs, into WCC while he was housed there. A hearing was conducted on September 6, 2019. At the hearing, Patient B denied knowing who had sent the drugs to him via mail. He was found guilty of the infraction and was sanctioned with 180 days loss of free recreation, 180 days loss of privileges, 75 days loss of good conduct time, 180 days suspension of visitation, 180 days restricted communication and correspondence, 180 days loss or restriction of store privileges, and one year denial of attendance at special events. He was also demoted to close custody. He did not appeal the guilty decision. The suicide note left by the incarcerated individual attributes his final actions to what he feels are overly harsh sanctions by DOC in response to the infraction, feeling persecuted for having a drug problem, and the loss of communication with his loved ones on the outside. The officer who discovered Patient B’s body was unable to immediately make a radio call for help because the batteries in his radio were dead. There was a delay of approximately one minute and 30 seconds before anyone entered his cell. OCO Findings: Failure of communication with incarcerated individual; delay or failure of emergency response Patient C had been in and out of a DOC facility numerous times since March 2018. Prior intake screenings documented a history of substance use disorder, attention deficit disorder, and hallucinations. At an intake screening on 8/7/2019, Patient C admitted to acts of self-harm and thoughts of suicide by hanging six months earlier; he also admitted that he had tried to provoke police officers to kill him. At that time, he was to be referred to mental health; however, there is no evidence that a mental health assessment was performed or that he was connected to community mental health providers upon release on 8/13/2019. A little over a month later, Patient C returned to the MCC Violator Unit on 9/20/2019. At this intake screening, he denied any mental health diagnoses and denied prior attempts of self-harm; as such, he was housed in general population. Unfortunately, due to the lack of definitive policies and processes in place for the violator population, Patient C’s prior records were not readily available, and intake staff was unaware of the prior history of attempts at self-harm. The following day, Patient C was found unresponsive in his cell, with a ligature secured around his neck. DOC staff initiated the facility emergency medical response, and EMS was called. Despite resuscitative efforts, vital signs remained absent and he was declared dead. OCO Findings: Delay in access to care; failure of communication between staff; failure to assume responsibility for the incarcerated individual’s care Patient D was incarcerated for the first time at the age of 73. He had multiple significant chronic medical conditions, including Parkinson’s disease and a cardiac pacemaker implantation. A Mental Health Appraisal in October 2018 identified Patient D as being high risk for suicide, and the records noted multiple attempts at self-harm. Despite this information, there was only one Suicide Risk Assessment performed on Patient D during his entire time under DOC jurisdiction, even though the records reflect many COA admissions as well as multiple documented incidents where Patient D was clearly exhibiting symptoms that demonstrated increased risk for suicide. In addition, the records demonstrate a substantial delay in care for Patient D’s Parkinson’s disease. This is a chronic, progressive disease associated with depression, anxiety, psychotic symptoms, and other neuropsychiatric manifestations; suicidal ideation is present in up to 33% of patient with Parkinson’s disease. At no time did Patient D receive a comprehensive evaluation of his Parkinson’s disease or the medications that he was taking for this condition. Patient D himself suspected that his symptoms were related to his Parkinson’s disease or the medications to treat it, and tried multiple times to ask for help – sending kites, asking the nursing staff, asking the psychologists, asking the psychiatrist – but no one took the time to bring the issue to the medical team or make Patient D an appointment, even when his tremors grew so significant that he had problems walking without help from other incarcerated individuals. On two instances, correctional officers attempted to bring Patient D’s motor issues to the attention of nursing staff, but again no appointments were made. In the days leading to his death, a unit sergeant took note of Patient D’s difficulty walking and gave him a walker even though one had not been prescribed (since he was never evaluated). Unfortunately, another sergeant took the walker from Patient D since there was no HSR for it. The DOC psychologist who reviewed this case believed that this action was the “last straw” for Patient D, and was the reason he committed suicide. Patient D was found hanging in his cell on 10/25/2019. There was a delay of approximately three minutes before the cell was entered, in part because an officer had to return to the unit booth to retrieve a noose tool for rescue. Then, after Patient D was declared dead, the body and surrounding crime scene were not appropriately secured per policy. Discrepancies were found between the timeline recorded by video and the timeline documented in the log book. Photos taken of the crime scene were of poor quality, and some evidence (a presumed suicide letter) was missing. OCO Findings: Delay in access to care; failure to recognize, evaluate, and/or manage “red flags;” failure of communication between staff; failure to assume responsibility for the incarcerated individual’s care; delay or failure of emergency response; failure to follow DOC policies Patient E entered DOC on 8/1/2019. Much of his medical record was redacted by DOC, so there was very little information made available to OCO regarding his mental health status. From the records that were available, several main risk factors for suicide were noted – including age over 60, history of substance use disorder, family history of suicide, and incarceration. Yet despite undergoing two intake screenings and a history and physical exam, these risk factors were not fully recognized by any of the providers who came in contact with him, and thus no referral was made for a complete mental health evaluation including suicide risk assessment. In addition, the intake screenings also found him to be edentulous and severely hearing impaired; however, despite Patient E’s Kite requests for dentures and hearing aids, he was not given appointments for dentures or audiometry until mid-October. Patient E never had a chance to attend those appointments since he was sent to Peninsula Work Release on 10/9/2019; unfortunately, those discharge papers do not reflect any efforts to connect Patient E to mental health, dental, or hearing aid providers. In the early morning of 10/30/2019, at a hotel parking garage, Patient E committed suicide by hanging. OCO Findings: Delay in access to care; failure to recognize, evaluate, and/or manage “red flags;” failure of communication between staff Analysis of Key Findings The two most frequent key findings were a delay in access to care and failure of communication between staff, present in four out of five suicide deaths. Delayed access to a medical and/or mental health evaluation with DOC or community providers partially contributed to the outcomes in these cases, since it is medically plausible that timely treatment of these individuals’ health care needs could have helped prevent them from choosing suicide. Furthermore, because of the failure in communication, healthcare staff were not made aware of the individual’s change in baseline behavior or their existing risk factors for suicidality, and therefore this key finding also partially contributed to the case outcomes. In the two suicides by persons remanded back to DOC, the agency’s lack of defined policies and processes specific to the violator population played a significant role in the communication breakdown. The violator population notably differs from the regular incarcerated population because of their short-term stay, and rapid referral for mental health assessment is vital. In three out of five suicide deaths, there was a failure to recognize, evaluate, and manage "red flags," which are clinical indicators of possible serious underlying conditions. This finding also partially contributed to the outcomes, since the individuals were not referred for the necessary mental health appraisals or adequately connected to community providers to receive appropriate care because staff failed to identify the existing risks of suicide or the individual’s basic needs to support activities of daily living (e.g. dentures and hearing aids). In two of the five suicide deaths, OCO found a failure to follow DOC policies. In both cases, a DOC Form 13-420 Request for Mental Health Assessment – required by several DOC policies – was not completed by staff who had observed a change in the incarcerated individual’s behavior; on interview, current and former staff members told OCO that they had never heard of this form. In multiple instances involving one case, a Suicide Risk Assessment was not performed by mental health providers as required by DOC’s Suicide Risk Assessment Protocol. This failure to follow pre-established policies and protocols resulted in missed opportunities to identify at-risk patients. A failure to assume responsibility for the incarcerated person’s care was also found in two of the five suicide deaths. In one case, although suicide risk was correctly identified by a health services staff member, the incarcerated individual was not connected to community resources upon release. In the second case, despite numerous pleas from the incarcerated individual and concerned outreach from correctional officers, health services staff failed to make appointments for a proper evaluation. Although it is difficult to determine whether this fragmentation of care had an impact on the outcomes in these cases, it is not consistent with community standards. Failure of communication between staff and the incarcerated individual was identified in two of the five suicide cases. In one case, the communication failure was related to overly harsh sanctions which, while consistent with DOC policy, was noted by the incarcerated individual to be the reason that he took his life. In the other case, although the nursing staff’s threat to deduct a co-pay each time the incarcerated individual called for help using the emergency call button may not have driven him to commit suicide, that harsh response demonstrated a lack of compassion and humanity for a mental health patient experiencing severe pain. Finally, a delayed emergency response was found in two of the five suicide cases, either due to non-functional equipment or the necessary equipment being located at a distant site. There is insufficient evidence to indicate that the outcomes would have been changed had the delays not occurred; however, the finding is indicative of an inefficient emergency response process. Additional Significant Findings Insufficient mental health outreach OCO identified a general failure to provide sufficient mental health support to DOC staff and incarcerated individuals. Some staff reported that they did not receive any outreach at all following an incarcerated person’s suicide; of those who did have contact with DOC’s CISM team, a few felt that the outreach was not enough. These staff members reported ongoing distress and occasional difficulty with the performance of their day to day work as a result of their experiences with these suicide deaths. OCO also found a failure to provide mental health support to the incarcerated individuals who worked or lived in the unit where a suicide had occurred. Several incarcerated individuals relayed the same feelings of sadness and trauma voiced by staff in the aftermath of a suicide in custody, but were not offered resources for support. Ineffective communication with family of the deceased OCO identified a failure to communicate effectively and compassionately with family members of an incarcerated person who had committed suicide. In one case, family learned of the death via a call from the coroner letting them know the body was there, but no additional information was relayed regarding the circumstances surrounding the death. In addition, family did not receive the incarcerated individual’s suicide letter until one month after his death; no copy was sent to the significant other, to whom the letter was also addressed. OCO Recommendations The following recommendations are pulled from the individual investigation reports related to the suicides. However, OCO’s primary recommendation is that DOC should convene a multidisciplinary, cross-departmental workgroup to review the suicides and consider not just OCO’s recommendations, but developing any additional processes or changes that need to occur to prevent suicides of incarcerated individuals in the future. Breakdowns in communication and/or documentation are a frequently cited issue leading to a failure to prevent the suicides and DOC needs to immediately and constructively find ways to break down silos and improve communication. Policies and protocols to identify those at risk • Develop health care policies and protocols specific to the violator population, including (but not limited to): o Updating existing intake screening forms to include family history of suicide, multiple ways of eliciting mental health histories, intellectual disabilities, and feelings of depression or suicidality1. o Implementing suicide screening at each point where a violator comes in contact with a staff member, since they can become suicidal at any point in their stay. Screening should include uncomplicated indicators of increased suicide risk so that correctional officers – who often form the first line of defense in preventing suicides – can participate as crucial members of the screening process. o Providing staff with very specific instructions on how to respond to answers that suggest suicide risk, with clear instructions on referring those who require mental health intervention. o Developing an organized record-keeping process, so that information is passed on to staff at a new shift, and can be accessed by staff during a future stay. o Designating medical and mental health staff who are assigned solely to the violator unit and responsible for all health care needs. o Requiring regularly recurring multidisciplinary team meetings – to include correctional, medical, nursing, and mental health staff – to monitor the violator population and discussing the status of those identified as being at risk. • Remind staff of the existence of DOC Form 13-420 Request for Mental Health Assessment, which DOC policy instructs staff to use in order to “report signs of mental illness 2.” o Consider clarifying these “signs of mental illness,” and include a change in baseline behavior as a potential risk factor. • Revise DOC policy and/or protocol to require the elevation of persistent declaration of medical emergencies by an incarcerated individual to the practitioner on duty and/or the facility medical director. This provides oversight of decision-making, additional accountability, and assurance that patients are not dismissed or overlooked. 1 Risk Factors for Suicide. National Institute of Mental Health, National Institute of Health, Department of Health and Human Services. https://www.nimh.nih.gov/health/publications/suicide-faq/index.shtml 2 Per DOC 630.500, “Facility employees will report signs of mental illness on DOC 13-420 Request for Mental Health Assessment to mental health employees/contract staff.” Safety of the physical environment • Change the emergency call system at all facilities to modify or eliminate cords, as more than 70% of inpatient suicides occur by hanging 3. Training to identify those at risk • Provide training to medical, mental health, and nursing providers on the risk factors, evaluation, initial management, and follow-up of suicidal patients. o Include refresher training on DOC Policy 630.550 Suicide Prevention and Response, the Suicide Risk Assessment Protocol, and the Suicide/Attempted Suicide Response Emergency Checklist, to ensure that these policies are followed. o Educate nursing staff on the assignment of initial mental health PULHES “S” codes and suicidal risk “R” codes per DOC 610.640 Health Screenings and Assessments 4. “S” codes must no longer be down-coded due to housing limitations. o Include Custody partners on the discussion of risk factors so they can be more attentive to the incarcerated persons under their care. • Provide training on compassion fatigue to remind staff – at the facilities and at Headquarters – that it is important for them to feel compassion for the incarcerated individuals in their care. o Review the overall therapeutic environment for all incarcerated persons, to ensure that they are surrounded by caring, empathetic staff who respond in a traumainformed manner. o Train all staff on ways to manage compassion fatigue. Prioritize the filling of all vacant positions with qualified employees or contract staff to minimize excessive overtime or the need to use less experienced staff for cross-coverage. • Provide training to ensure that providers have a better understanding of certain diseases, so they do not overlook “red flags.” 3 Williams SC, Schmaltz SP, Castro GM, Baker DW. (2018) Incidence and Method of Suicide in Hospitals in the United States. The Joint Commission Journal on Quality and Patient Safety, 44, 11, 643-650. 4 Per DOC 610.640, “initial mental health PULHES “S” and suicidal risk “R” codes will be assigned. Patients with emergent needs will receive clinical follow-up.” o Offer mandatory training on Parkinson’s disease to Medical, Mental Health, and Nursing providers. Include Custody partners on appropriate sections so they are familiar with the signs and symptoms of Parkinson’s and other dementias, so as not to misread these symptoms as willful aggression. o Offer mandatory training on the evaluation and management of falls and syncope to Medical, Mental Health, and Nursing providers. Referrals for internal medical and mental health care • Eliminate barriers to medical appointments by implementing a clear policy and procedure that ensures an appointment for every patient who requests one. • Require an evaluation by a physician or advanced practitioner within a week after a declared medical emergency, to ensure that adequate treatment has been provided and appropriate referrals have been made. • Review with custody and medical staff the proper use of emergency restraint chairs. o Train staff that patients who are found unconscious may be disoriented and instinctively defend themselves when finally aroused; they should not be placed in restraint chairs, but instead should undergo a medical evaluation. • Ensure a follow-up appointment any time a new medication is prescribed or dosage of a current medication is adjusted. This is not only reduces poor quality and erroneous prescribing 5, but enables the provider to assess for medication effectiveness or to make adjustments as needed. • Develop additional methods and resources to reduce the risk of suicide in the incarcerated population, including use of other incarcerated individuals as peer support to help with feelings of isolation. Continuity of care upon release • Develop a policy and process for connecting patients to community mental health practitioners upon release from a DOC facility, including transfers to work release centers. 5 World Health Organization. WHO Global Patient Safety Challenge: Medication Without Harm. https://www.who.int/patientsafety/medication-safety/strategic-framework.pdf?ua=1 Emergency response • Strengthen current policies and procedures so that rescue occurs promptly; dictate specific response times to ensure that delays in rescue do not occur. o Improve accessibility to rescue tools by locating them in the officer booth on each floor. o Require DOC staff who distribute and/or carry radios to ensure that the batteries are charged and the radio is in good working order before shifts begin. Communication with staff, incarcerated persons, and loved ones • Ensure that all documentation in the chart is legible, since clear communication among all providers involved in a patient’s care is imperative for good clinical outcomes. Ensure documentation quality via clinical oversight at appropriate intervals. • Implement a clear policy and procedure that requires response within 24 business hours for all medical Kites containing appointment requests, and within three business days for all other health-related Kite communication from the incarcerated population. • Revise DOC policy related to permanent restrictions on communication with loved ones for any reason, including contraband conveyance. A more compassionate policy would be to impose timeframes and provide clear pathways back to communication. • Implement a trauma-informed approach to informing family members of the death of an incarcerated person. o Family should receive a letter from the facility or DOC leadership expressing condolences, providing any immediate information that can be released, identifying a person at the facility with whom they can speak or in the alternative, notifying them that all critical incidents such as suicides are reviewed and that they can receive a copy of the report through public disclosure, and including a full inventory of the person’s property with information on how to obtain it. o Letters left by the deceased person addressed to family members should be expedited for review and released to all identified persons, as feasible. Support for staff and incarcerated individuals after a suicide • Develop sufficient internal resources or links to external community-based mental health services to ensure access to mental health personnel • Ensure mental health assistance for all staff either directly or indirectly involved in the care of an incarcerated individual who has died by suicide. After the initial CISM contact, connect staff with DOC psychologists for referral to community mental health services for ongoing support. • A suicide in custody can also have an impact on the mental health of the population within a housing unit. Provide mental health support resources to incarcerated persons who lived or worked in the unit where a suicide occurred.